good afternoon everybody and uh welcome to this summer from a beautiful
afternoon in liverpool how very unusual it is to use that sentence
i’m peter winston lee i’m standing in for hillary ransom who has been coordinating the ref
submission for the school and this seminar is part of a series
which was set up to celebrate impact case studies which are part of the ref submission
ref submission on the 31st
this is one of eight submissions of course it’s terribly important to
bear in mind that even if the ref didn’t exist the liverpool school of tropical medicine
has as part of its core values the need to make impact and improve health
in particularly in low-income countries and um at that i’ll hand over now to bert
squire who is going to be the master of ceremonies for the rest of the seminar
and we’ll handle questions toward the end over to you bertie thank you very much
peter and welcome everybody um just to say a little bit more for those who don’t know who are
listening who don’t know about ref ref is the research excellence framework which is a mechanism that we have to report to as
universities in the uk my name is bertie squire i’m a professor
here at the school of tropical medicine i’ve been working for 25 years in tuberculosis i’m also
dean of clinical sciences and international public health and it’s a delight that we we are able to share some of the
highlights of some work that we’ve been doing in the in the recent years i do want to say a few things on
housekeeping please do post questions and comments in the question and answer function
on teams throughout the seminar we’ll see how many our panelists can pick up as we get
further through as we get towards the end um i just want to explain the running order we’ve got
three lstm speakers who’ll present a series of slides for about 20 minutes and then we’ll move into a 30 minute
commentary from five panelists who will each introduce themselves in turn from
different parts of the world and and then finally the recording of this seminar will be
available on lstm’s website tomorrow so if you if you’ve got colleagues who
miss this um they can access it again tomorrow so um
as you know uh today is world tv day and we’d like to share some of the
highlights of work that we’ve done at lstm in relation to multi-drug resistant tuberculosis
and this is work that’s contributed to changes in who guidelines for the management of drug resistant tb
i’ll be joined in the presentation by lstm colleagues ewan tommeny who’s a systems modeler
and lara rosso who’s a health economist um i please do tweet as the seminar
progresses there are a number of hashtags and um and
twitter handles at the top of this slide which should appear in the in the q a for you shortly if they’re
not already there and there’s also a link to uh the website where there’s more detail
around some of the things that we’re going to be talking about today including references to the published
work that sits behind behind this so here’s the running order
i’m going to say a little bit about tb in general for those who aren’t so familiar with the uh with uh
tb and the global burden of the disease then you and i’m going to introduce something
called the tb care pathway which leads into you and talking about virtual health system modeling followed
by laura talking about work on shortening the duration of mdr tb treatment
and then it’ll come back to me to talk about shifting to outpatient management of mdr tb
and i’ll end with a few conclusions before we move into the panel commentary
so before we get into some of the global burden of disease i thought i’d share a few things on drug resistant tb um just so
that we’re all all on the same page about some of the words and nomenclature that will come up
as we go through so treatment for drug sensitive tb requires four different drugs last
six months as a standard if the infecting strain is resistant to
one or more of these drugs it’s termed drug resistant if the infecting strain is resistant to
the key drugs with famicin and ison acid it’s termed multi-drug resistant and the most widely available test for
drug resistance today uh gene expert a molecular test only detects resistance to rifampacin so
rifampicin resistance is taken as a marker for mdrtb
six years ago the most commonly recommended treatment for mdrtb required more than five drugs and
took 20 to 24 months to complete and it included around two months worth of
daily injections so that was the starting point for the work that
we’ve been engaged with along with a whole series of partners as you’ll see as we go through
when we think about it’s worth just pausing and thinking about the burden of disease from tuberculosis
the latest data until the 2021 global tv report comes out um
our figures are numbers from 2019 so 10 million tb cases approximately of which 350
000 were termed multi-drug resistant and at 1.2 million tb deaths and the incidence and
mortality which goes with it really it shows a burden
in the lower middle income countries on this map of the world you’ll see the darker
blue areas are those where the incidence is the dark blue purple is more than 500 per hundred thousand
i’m also sharing on the right hand side of this screen a graphic which gives you the age
distribution so this is a disease that affects all ages and these are the global
numbers and the other point of this graph is to clarify that males account for more than
half of the estimated 10 million people who develop tb annually and they also account for two
out of every three crazed cases which go undiagnosed or untreated and that maps through into the mdrtb
population as well the white on this graph are undetected cases
the green are males and the purple females a few words on
progress towards targets now there are massive targets related to tb control set by different relevant
international bodies i’ve picked a couple one here is from the un high level
meeting which took place in 2018 and set a target
for the completion of 1.5 million treatments for multi-drug resistant tb
cases and you’ll see that in 2018 and 2019
we achieved only 22 of that so we’ve got a year to go to fit the rest of that the other target
i’m going to share here is one from the world health organization’s ntb strategy it has a strategy for reducing
the costs faced by families affected by tb households affected by tb
and it uses a term called catastrophic costs the target is that no
households affected by tb should face catastrophic health care associated costs
and you’ll see here from this for people with drug resistant tb
um the data so far shows that more than 80 percent are incurring these catastrophic costs
the catastrophic costs for the tbe community is occurs when a household incurs more than 20 percent
of its household annual spends more than 20 of its household annual income on
healthcare associated costs related to tb
in these times uh we do need to make mention of kovit19
it will be no surprise to anyone that notifications for and and uh enrollment into tb treatment
which is the best way of combating this disease both in terms of reducing morbidity and transmission has
reduced substantially in all countries these are the four of the
highest burden countries and you’ll see reductions in tb notifications of around
50 over the um first few months of last year
and the world health organization estimates that the impact of that reduction in case
detection will result um in substantial increases in tb mortality so the blue
lines i’ve put on this graph on the right show that a 50 reduction for a duration of three months
in a given will result in around 0.4 million extra tv debts so finally before i hand
over to ewan it’s important to think of access to tuberculosis along a continuum
um starting with the onset of symptoms recognition of those symptoms by health
services health systems testing for and confirmation of tuberculosis using different diagnostic
tests which i’ve listed here getting those tests back to patients getting treatment started and then
monitoring that treatment right through to cure and completion and it looks like a really
useful a nice linear pathway but as everyone will know um that pathway it takes a while
and sometimes isn’t quite so smooth so just the last couple of points on this
you and i think i’ve given you control so i’m going to let you take over the first part of the of this
pathway is where uh ewan is going to uh speak and uh
uh really around operational modeling health systems modeling for mdr tb and then the the latter part of
the pathway is where laura will talk about shortening mdr tb and i’ll talk about shifting to
outpatient management of tb over to you yuan thanks betty
good afternoon so i don’t have a huge amount of time to go into a lot of detail here but i want to give a brief overview of what we mean by virtual
health system modeling outline some of the key characteristics of the models themselves and then give a couple of examples of how we’ve used
these in evaluating strategies for the diagnosis of drug-resistant tb so on the right here of the slide you
can see a couple of screenshots from a model showing various parts of the patient pathway the key thing to highlight in these
models is that when we run them we actually see the people moving about the model traveling along the pathway just as they
would in real life so leaving home chewing at health centers being tested all the while incurring various costs
so these models are incredibly detailed and able to represent the often complex pathways that patients take and
capture bottlenecks and capacity constraints along the pathway critically they have this visual
component now this is particularly important because it means that we’re able to engage non-modelers
in both the development and the validation of the models quite unlike what we might term as black box modeling which is all a bit more
opaque and we find that they certainly can help in both the understanding and the trust then of the ultimate outputs we’re also
very easily able to answer these flexible kind of what if questions so flexibly so for example if we were to
wonder you know what if the prevalence was higher what if we had a broken x-ray machine at this particular health station uh what if we had fewer nurses
or a stock out of some important diagnostic resource such as expert cartridges and these
could all easily be answered um and just again then as lots of data go in we get a huge amount of data out
the other side so we can kind of output this directly from our modeling software witness to excel where we can then conduct our
statistical analyses and finally just to say that these models are incredibly powerful so we can simulate about 10 years worth
of real-world diagnostic processing time in under under a minute on our on our
computers and very briefly before i move on just to briefly explain why these models are
particularly necessary and indeed helpful uh building them in this way rather than say in some other you know
um software such as excel um you know each diagnostic site is unique and we typically have many options or
strategies to choose from so particularly focusing on these capacity constraints and the bottlenecks
in our health system is critical and we’re not only interested in how these changes would affect the health
system but also the patients which i’ll talk a bit more about now
so this here this is a visual from a study in philippines and sticking with this point about patients this is the journeys that
patients take in a typical site in order to get a tb diagnosis this is before the introduction of
gene expect technology so using microscopy and it highlights really just that the simplest way to get a diagnosis
requires four trips minimum now these trips this is you know the very simplest um journey a patient
might take often there’s many more journeys on top of this but these trips require you know time off of work often
maybe a patient might take a day off of work and so that it’s not as simply a case of the patient walking to a health center
and getting their diagnosis even at the minimum it’s four trips and often we found increasingly many more than this
and so i suppose my point from all of this is that any changes to diagnostic strategies should really consider patients
centrally to this decision making and you can see here i’ve just included
a couple of the details from well some of the figures so while tb patient costs are high for all patients
particularly so for drug resistant patients these are particularly higher so you can see here this is 2 256 on
average for mdr tb patient throughout the course of their diagnosing treatment in philippines and this catastrophic cost indicator
that bertie mentioned well for drug susceptible patients at 28 we found 80 percent of drug resistant patients
were incurring catastrophic costs so in order to kind of build these
models firstly when we’re evaluating new strategies we need to understand what’s happening currently or our base cases return it so in doing
this we take inputs for a number of different sources and we establish the pathways through discussions with programme staff
health workers patients and then these draft pathways often which have many iterations before we’re confident
with them we can then build from to look at changing and for new strategies
so typically we use an excel interface we take all of our data put it all into kind of nicely managed
tables in excel then we run this through our software which is we’ve been using witness for many years now
i’ve just included here a little list which shows witnesses used in a variety of different
sectors but we’ve found it’s particularly great for modelling patient pathways and can really capture all of the
the complexities that are found here [Music] so this final slide here is just to give
an example of three slightly different key studies which we’ve conducted using this modeling approach for mdrtb
diagnosis um firstly at the top here this is either langley study in tanzania this is an integrated modeling approach
which included both diagnosis and transmission and then in brief they identified that a further i think 1285 otherwise missed
hamstring assistant cases would be picked up by changing to the optimum strategy the next study in the middle here is our
work in the philippines so we collected primary data from many sites and we predicted a considerable increase in mdr
tb detection from the rollout of expert and this increase has ranged depending on the
site from about 20 to 200 so quite variable and finally uh laura is about to talk to you in a moment
about our work on the stream trial which we’ve also conducted some virtual health system modeling um including both
again health system cost and patient costs thanks erin um hello everyone and thanks
for joining this session today uh as bertie and you have already mentioned today i’m going to talk about
the shortening of multi-drug resistant tuberculosis regimen uh mainly about the economic evaluation
of the stream trial so i’m going to start by presenting the
clinical context first in 2011 before stream who was recommending a 20 to 25 uh months
regimen and this was based on very low evidence and despite the high tb burden
stream is the first ever multi-site multi-arm multi-stage phase 3 randomized control trial on the right
hand side you will see the kaplan myograph which shows that the time to unfavorable
outcome did not differ significantly between treatment arms in the modified intention
to treatification efficacy analysis favorable status which was defined
by two negative cultures at 132 weeks after randomization and at the previous
occasion with uh now intervening positive culture or previous unfair outcome was reported uh so efficacy uh so um
the federal stat status was reported in 79.8 participants in the long regimen
group and 78.8 participants in the short regimen group so a difference of just one uh adjusted for hiv status
of just one percentage point final stream clinical results have been
published in new england journal of medicine in march 2019
stream was also the first to include within a trial economic evaluation so we’ve collected patient and health
system cause data to investigate the nature magnitude and timing of the changes in costs
we’ve also showed that the short regimen led to substantial savings for both participants and healthcare system
despite the additional required ecg monitoring for those on the
moxifloxacin arm on the right hand side of the trial of the slide sorry you will see a photo i took
it and this is a booth a bank owned by bank where patients had the
possibility to loan money from and what actually made me took this photo it’s because it was
in a parking lot in a tv hospital in
delhi um in terms of health system costing we’ve showed that the short regimen reduced
health system caused by 20 in ethiopia and 25 in south africa most of the cost saving 61
occurred in the continuation phase in ethiopia and 85 in uh south africa we’ve also conducted
a probabilistic cost effectiveness analysis uh that showed that the short regimen has a probability of being cost
effective of above 95 if their willingness to pay for each additional favor outcome is less
than uh 19 000 usd uh used dollars in ethiopia and 14
500 in uh south africa
there are further savings in terms of uh patient costs so in ethiopia the
transport and food cost saving for attending the assessment visits was
thirteen us dollars um and in south africa this was 64. in terms of supplementary
expenditure participants on the short regimen in ethiopia reported reduction of 225
u.s dollars per participant and this is graphically represented on the right hand side of the of the slide you
will see that uh the cost savings start happening even before a treatment end which is at week 44 those on the
short regimen and even before the uh end of the intensive phase which is week 16 for the
short regimen also participants uh additionally participants on the short
regimen reported additional hours worked compared to those on the long regimen and this was about five hours per week
for the 132 weeks duration of the trial and as you can see
in this graph patients on the shorter regimen started work work early and worked longer hours compared
to those on the long regimen this is represented by the darker red beats
on on the graph the health economic analysis was published in may 2020 in the
bulletin of double ho the same health economic methodology is
currently being used in the short research package developed by tdr and who
and is currently used in ben indiac nigeria and pakistan to
support the rollout of all oral outpatient regimens the preliminary health economic
and clinical results have been presented at the who guideline group in 2018 the stream data um
contributed to the formulation of two wh updates on management of mdrtb in 2018
and to the 2019 who consolidated guideline so as i’ve just mentioned this was one
of the updates in 2018 then the consolidated guidelines have been uh released
stream trial is mentioned several times especially because it improved the
certainty of the estimates and the health economic results are also being mentioned especially the
earlier return to work for the patients and the reduced cost of the shorter regimen
thank you very much thank you very much laura and
also much gratitude to usaid and lots of our other funders
so the last bit of what i’d like to what we’d like to share here is you will have heard now that um we
have ways and means of improving access to diagnosis for mdrtb
of improving duration of treatment and that both of those are
useful are beneficial for patients the next question is where do
patients receive their medication and when we when you’ll remember i
mentioned that early on in mdr management we always required people to have daily injectable drugs
um danielle cohen one of our welcome trust uh clinical phd fellows uh back in
in the in before 2015 actually did a trial moving towards delivering injectables
in the community so long-term injectable drugs although now we are moving to all
oral treatments for drug resistant tb they were essential and they remain
important for some forms of drug-resistant tb and we’ve always uh we’ve all in
community-based management has always been encouraged but of course daily injections are difficult to administer
in the community and until this work most models of community-based treatment
really resulted on health facilities health workers going to community members into going to
see patients in the community or expecting patients to travel to the health facility
um colleagues at the ministry of health national tv program in malawi did alongside um danielle
was an individually randomized pragmatic trial where patients either received their injectables for
the first two months in hospital or at home delivered by a lay guardian usually a family member
who was trained to deliver the streptomycin injection results of that a study had published in thorax and i
just wanted to share very briefly the economic outcomes of that the um the
clinical outcomes were equally good in hospital-based and community-based management
but the uh biggest effects were in the impact on on patient costs so
patients saved money by by this mechanism and both patients and
their carers saw these substantial changes also um this slide shows that the
proportion of trial participants who incurred catastrophic costs during treatment for drug resistant tb and you’ll see
again community-based management uh led to a substantial reduction as i said earlier i described
earlier catastrophic costs um are an important indicator for the
ntb strategy and the who definition that we work to is a threshold of more
than 20 um incurred costs relative to household income
uh 10 uh uh cost healthcare costs incurred
we know results in substantial economic and social consequences for households making it very difficult for them to
recover and at a 20 threshold we know that there are adverse outcomes associated with tb
as well you’ll notice in this slide that the proportion of both men and women with mdrtb who incurred catastrophic
costs was around 60 for those managed as patients compared to only around 10
for those managed at home and both men and women appeared to benefit equally from the
home-based management so this last slide here gives a range of
acknowledgements for collaborators for this part of the study we haven’t
shown the huge range of collaborations for all of the other work that lara and euan have presented but this is
an indication just within this one study of the kind of of wide collaboration we’ve been lucky
enough to have and the photo shows uh one of our one of the tv program
one of the tb ward nurses training um the household members
lay carers to draw up and deliver the injectables and incidentally safe
safely dispose of them as well so in summary uh
we’ve had an impact with a load of partners in in showing how health system modeling
can facilitate rollout of new diagnostics including detection of drug resistant disease
we’ve had a role in showing that the shortened
tb regimen tested in stream has already benefited more than 200 000 people
through the 82 countries where it’s been adopted with an overall societal cost saving of an estimated 357
million us dollars in 2018 and if countries now shift to outpatient
home-based management of ndrtb either because we can now shift to all
oral regimens um which now contain the new drugs such as the d’aquiline or because uh
home-based injectable delivery is possible it this should result in further reductions
in cost for patients and health systems and as lara mentioned and i hope corinne
male will pick up this economic evaluation of of those potential impacts will be
captured through the short operational package which is facilitating that rollout
and the crucial factor in all of this is the importance of saving time spent at health facilities both for
patients and for uh health systems and with that i’ll say thank you and
move on to our panelists so robbie could we have the slides off
and i’m going to hand over first to charles to charles go ahead to introduce
yourself and any thoughts triggered by what we’ve been discussing
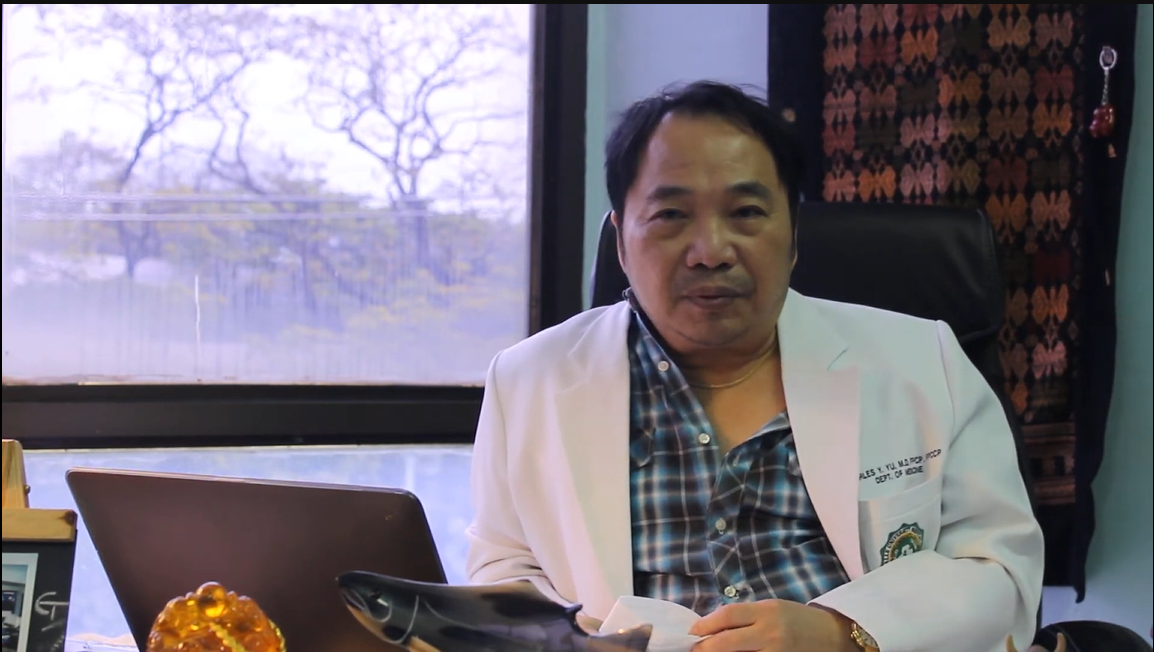
hey everyone thank you bertie i am professor charles yu i’ve been working with the liverpool
school of tropical medicine since 2016. uh it’s been an interesting time
and our the work and collaboration continues up to this time
i can relate with all the three presenters one for u1 because we had this creation
of the journey of the patient pathway in order to create the model and one of the outputs of the project
was actually a paper on patient costs and i’d like to say that we have the only local
published data on the catastrophic cost of the ds and mdrtb ours is
exactly 80 percent of our mdr has catastrophic uh losses and 28 of the s what was
interesting in the findings was that of course the majority was due to lost productivity i think
which is uh echoed all over the world but one of the third leading causes was supplements and
vitamins vitamins uh in the british violence and so the other one is uh in the cost of
travel and medical costs and when i presented this uh yesterday
through the first research forum of our national tv program uh there were only four presentations of
heated papers and many of the reactors across the country were impressed and actually described the
project as illuminating in in the sense that it opened the eyes of many people on some of these
treatment uh costs the other thing that we can also uh relate with is
laura’s uh the the stream trial because we are currently doing uh the the all oral short course mdr
arrangement in another project and and this was happening in the covet era and we could actually see
that we were not losing patients despite the fact we were strict lockdowns and uh we combined the use of
community-based workers which we had trained called which again relates to bertie’s
uh presentation and the innovations that had to be done because they couldn’t
travel and do the partnering with the patients but we used a lot of social media and and cell
phones and devices we could even compare our results with the video as instead of vot
regiment and we could actually show that the results of the community-based health workers were in fact
better uh 90 percent diverse 70 versus the video observed treatment
which was actually uh surprising to us now uh i’d like to say that uh most of the partnership with
lstm which continues by the way where we’ve been asked by the national tv program to look at
a problematic region and to see if active case findings can actually improve the
case detection rates or the pace notification rates of course now again the copied laptop very very challenging
to even travel uh to those places but all the work that has been done with in
partnership with lstm and as a result of the work of lstm uh worldwide is
impacting on my country in uh where kovid is a i guess a obstacle but but i think
with the learnings that we have developed at least we know where we’re coming from and we can measure
ourselves for example measuring whether we could reduce the catastrophic cost when shifting the community base will
actually lead to real economic uh savings
as well as the shorter regimen which means i think the quality of life of our mdr patients are much
better so this would not have happened i’d like to thank uh bertie
[Music] uh laura you and because we were strangers to the mathematical modeling
technology but you can be proud that five years after you actually have local experts there’s been a successful
transfer of technology where our own team of young scientists are
applying the models with assistance from un and aura but applying it to our ntp
partners and that is the ultimate evidence that we can have a successful transfer of technology
and transfer the google degree of modeling into something that policy makers can
understand thank you thanks thank you charles very much indeed that’s super um
i’d like to move on then to sarah sarah would you mind um taking over
introduce yourself and any thoughts that are our overall presentation triggers thank
you very much bertie i i was in the wrong place earlier i was having kittens because i i was i was looking at
it as a as a viewer rather than as a panelist um so uh yes so i was
this is really i suppose a question to in a sense to all of you and you may all have a different perspective
on this i uh sorry i should introduce myself um i i i’m sarah meredith and i’m uh
i’m the clinical chief investigator on stream um and have uh had a delightful
working relationship [Music]
apologies okay so uh yes so i i’m i’m i’m i work on stream so my question
was uh to think to all of you um to what extent do you think
um the the uh getting the obtaining of the the
uh views um and and weights in terms of your analysis of uh
of participants um is i mean how so a how would you do it
and b how is there any value in it ewan mentioned it in relation
to his to the um the diagnostic modeling
uh but i know that uh lara uh which in her presentation is has been
the focus has been very much on the amount of money saved and as a as a simple trial is that does seem a very
important aspect but i was wondering if there are if there is room for for for for more
nuanced um ascertainment of of of participants values in this
thank you sarah very good question what i’m going to suggest is that we hold that question
get to hear from all the commentary if that’s okay i know lara probably is best suited to
answer that one a little bit further on down um because there are some plans i think for getting some more information on
that from the stream but just in the interest of time i’m going to to say thank you for that and move and
move on to uh dr narendran um also involved in stream trials
welcome and do introduce yourself and any thoughts you have on impact where this work is going great
[Music] uh thank you dr bertie it’s indeed fortunate to work with sarah
andrew the entire team of lstm lara langley jason
i have to rightly acknowledge all of them because it was really delight because i chose
medicine because i was weak in mathematics then found out that finally i had to land up with statistics and all this stuff
so the hard way to learn so the the main crux of the point is that
uh what i i admired with the lstm group was trying to get the details of
indirect cost see getting the direct cost is not a very big issue because you know that you are spending so much of money it’s just
a question of addition summer subtraction multiplication but getting the indirect cost using very
specific questionnaires used in stream i was really impressed with we were not part of the stream stage one because
that was the revolutionary study i should say because if you look at the parameters
with respect to outcomes with respect to toxicity with respect to death all of them are non-inferior
any statistician will here in the group will appreciate but the economic cost was superior there was a
superiority if you can analyze where you can definitely judge only with that
parameter in stream stage one others are all non-inferior that is the shorter regimes compared to the longer regiment
but compared to cost effectiveness compared to the way it can be practically
put into the field as a translation it was really a superiority design or a superiority
which was established and the who and our national program was quick to realize that and that’s how
we got the shorter version of the regimen in mdr tv the stream stage 2 is much more complicated analysis which
you people know better because you have shorter regimens of varying durations and now you are focusing yourself to
what you means a decentralized healthcare system which is very very important especially in the context of corona
because as you rightly pointed out on there charlie also told the time spent
in health facilities actually takes a lot of indirect cost which we all know that’s
very very important and the other aspect is the lockdowns and injections they don’t go well with each other so we experience
this in steam stage two when we when you try to reach their houses even then it was very difficult for us to
give the injections because there was always a stigma of tuberculosis still lingering in some of the places
so the people are much more comfortable coming to the hospitals for injections rather than and how do you manage these
when there is a complication due to an injection of course all of them are already treated so those problems will always be operated
when you have a oral regimen and the only the only point of caution
is that when you are using newer tracks like binocular in other drugs we have to be little careful at
least in the initial phases that the patients are tolerating these drugs so the way in which we have to
decentralize it may be a little uh you have to go through a methodological and meticulous way so that we are able to
teach the attenders to to uh to initially itself find out problems if they arise it’s not that
these drugs are quite safe we know that now but uh it’s always we have to take it with a pinch of salt anyway i’m really grateful
to the funders as well as to mrc uh it was really a enjoyable time
working with you and hopefully we will from nirt my greetings from our director and our dgi
cmr so we will try to collaborate with you in future and it was really exciting to be in this
uh conversation with all these tall ones thank you thank you so much
sorry thank you so much dr narendra and that’s really really helpful and um i’m going to just hand straight
on to uh corinne corrin would you mind um
introducing yourself and some thoughts hi many thanks for for
inviting me to celebrate the tv day with you um i’m coinman i’m
from the debate show and special program that is called tdr which is for tropical disease
research and uh our work um at tdr focus more on
operational implementation research so the the the last uh stream of the of the
research path and and i’m very pleased by all the work we have heard um that was led by the
lsatm because uh we use that uh hugely um for especially for a program uh that
we have developed that we are leading with our colleagues from the global tb department where we have developed a
research package for um helping country to use short all oral regimen same regimen that
you you have heard about in the stream trial but uh to try to
to help this country to use the new drugs and and to do it under operational research condition and what is very important is
not is that this can this country need to of course um look at the effectiveness of this uh
short haul or regimen in their settings but also other parameters and and then of course we proposed
to them to to look at quality of life the impact of the quality of life the feasibility the acceptability by the
patient but also the cost because at the end there are some decisions that need to be
made by the by the country on going for a perhaps a treatment that
is a bit more expensive but because shorter at the end
made saving not only for the program perspective and but also for them from the patient perspective
and if you think about it with the with the new drugs that are currently developed then there will be
more and more choice by the national program to go for one or another regimen so
this analysis this uh economic analysis and economic arguments will be more and more important and the
methodology that you have developed for the for the stream trial is really something that we can use and
then democrats democratize and and and propose to more country currently in the short program there are
um 25 countries that we are helping supporting a few of them used uh the the package
that is on economic cost because as you said it’s say it seemed like something complex
but more it goes more we can democratize that and more we can reach um more and more
country to to use this and to and to have argument economic arguments
so i’m very pleased by all the work you have done you simplify your life and uh and it’s not finished we need you
for a lot of more studies thank you thank you corrine very very kind words
thank you very much indeed very helpful and um one thing i just wanted to bring out is one of the
great things about the linkage with tdr and who has been the as you nicely put it
democratization of this approach and especially through to the francophone countries and and your
your work through the west african tv research network warren tb and the central african
research network has been really invaluable and i think bringing some of the perspectives around
the importance of costs to patients particularly but systems as well is has really been very helpful i’m going
to hand over now to jillian um to introduce yourself julian and any thoughts
hi can you hear me my signal um died for a little while but i think it’s come back um
now well thank you so much so i should say i’m talk to jillian turner um i’m currently working for the foreign
commonwealth and development office as a senior health advisor and um based in pakistan leading across
health and education programs um for me it’s just fascinating and um it’s
like a returning home to to be a conference on tv because that’s
where my research was based before but what really strikes me from the presentations
an understanding of patient perspectives is in terms of um designing not just
tb programs but also any um any any care interventions where
patients need to have a significant interaction with the health system on a frequent basis and and i think it’s it’s wonderful that
this research has been taken forward and has had such impact in the way it has
affected mdr treatment regimens but i think there’s you know that there’s more that can be done with those lessons as well
i think it’s great that now in the sdgs there’s a recognition
that patient costs and particularly catastrophic costs need to be a measure of how well we
collectively are performing in global health health in terms of meeting patient needs um but
i still think that you know we we still see that the way those are collected it’s it’s challenging it’s time consuming but
i think what you’ve done so well is to be able to take a tool and have it stand standardized and systematized
so that it can be used in different settings as well um and it’ll be great to sort of
see how collectively as a global community we can take that forward into other areas of research also
um i think the other thing that i really want to reflect on is if this is about
time the title of this is about time and it is about time that we have had better um tb treatment
regimens and also that we understand patient needs better but it’s also a recognition of how long
it takes to do this kind of research to get it into policy as well so i mean i can remember working on
patient costs back in 2001 um and sort of the time it takes
to conduct the research in the first place to make sure that sufficient evidence is available to be able to convince policymakers but
but also then sort of getting that into policy translation and into practice i mean i see in pakistan
now that some of the um interventions on drug sensitive tb that were recommended
by five sometimes ten years ago are now being implemented but it has
taken a really long time to get them from guida from guidelines into routine practice and even now some
of those things are not seen as routine they’re seen as exceptional in some circumstances um so just the a real kind of
encouragement i do think this is really really critical um the other thing that just strikes me
is that the more we can do to accelerate patients access to an effective
diagnosis and to get through treatment um not only reduces their time and course which is
critical particularly for the poor whose um sort of uh discretionary resources
are so much less but also in terms of overall overall disease control globally because the longer it takes people to
kind of access the care they need the longer those disease circulating in communities and um the more it impacts
others and i know i’m speaking to the converted there but um thank you happy to answer any questions
if needed thank you very much jillian that’s
um a lovely uh a lovely way to round up we’ve got a few minutes left so if anyone’s got comments that they want to
post in the q a please do and meanwhile i’m going to return to sarah’s
question um and and sarah i hope i’m going to get it right but you were you were saying we
we were we were really focusing in the stream in collecting costs and you were thinking about is
there a more nuance are there other perspectives we need to be thinking about and maybe i could hand over to lara to
say a bit more about that because i know in stream one we were very focused
on direct patient costs indirect patient costs but stream two methodology which is the next
phase of the stream trial has more in it in its own right and nested within it i know
lara and colleagues in uganda have been working on on more over to you lara yes
uh thanks verity um yes so you’re right um we are planning to
conduct a qualitative study just in uganda to understand more about the patient perspectives for example in
stream one we showed that patients were spending a certain amount amount of money on supplements but we’ve we’ve we had no idea why
necessarily because the clinicians were recommending the the supplements to them was it because they
they felt the need to do so so we’re trying to explore this more through this uh quality study
in uganda and um there are also some other sub-studies we are currently doing especially in um
two uh two uh models we are currently building where so in in the stream one trial
we’ve collected data on how the patient pathway looks like in the stream trial and now we’re going
a step further and we’re trying to see how we can amend that patient pathway to make it more patient patient-centered
to reduce the cause for both the health system and the patients without um
without decreasing the uh treatment efficacy so um yeah these these are the
the two things where we’re currently doing in uh stream traditionally and we’re also collecting the uh quality
of life data which which is uh important uh as well thanks lara
um lovely to shout out now for brenda mungai posted i think from kenya
i know the team there have taken forward the health systems modeling um for more general lung disease to sort
of think about the way in which active case finding for tb may have additional spin-off benefits for other
parts of lung health detecting other lung diseases um and actually in the in the first iteration looking
like it’ll detect cardiac problems as well but the team there is really
in just beginning on that pathway so great to hear from them um i’m just going to i’m conscious that
we’re probably coming to the end of our time here um i’m just going to
pause a bit to see whether there’s anything more coming through on the q a which there isn’t at the moment
um so sarah i’d rather cut you off with one question so i’m going to come back
to you as a fellow stream investigator whether there’s anything more you’d like to
to to say thank you very much well um that that
that comes as a bit of a shock to me um no i don’t think so i mean i i it was
this um i mean you know the the issue of of cost you know for for you know for so
far so many of our our patients and and communities they you know that
you were clearly easily getting into the catastrophic costs and and that and so in itself you could
you can see that probably anything that um that that that shortens treatment pretty much
anything that shortens treatment unless it really um makes people feel very unwell
um is going to be of of economic benefit to them but but it
it was this issue of you know in there is this assumption that everyone
is in that situation and not necess everyone isn’t necessarily and so just just you know how to
how to make this analysis potentially more more able to reflect
different different values in different communities so i thought that was very interesting so i i was i was
very pleased to hear what you’re what you’re planning to do laura um and i i um
i mean just the question for bertie really then so do you think my reductionist view is
is probably you know is it is it sort of dismissing
all of your your years of work because obviously it’s going to be cheaper if it’s uh if it shortens so it shortens
treatment for people yeah i’m glad you brought that i’m glad you brought that up sarah
let me round off by just um answering that a bit so you you i’m going to ask everyone just
cast your mind back to lara’s slides what was interesting in stream one is that
patient costs were were already less in the short regimen at the same time as they were um
as in in the bit where they were also being compared with the costs in patients on the longer arm so
if you just concentrate the analysis just on the time when both groups were on treatment even there there were savings so people
were returning to work even before they’d finished treatment more frequently in the short regimen so it’s really
important to understand that and the other thing was and this is what sarah lara was pointing
out is that patients were spending less on other things so nutritional supplements and
the like and charles also mentioned those so there’s something else happening that’s not just about duration and i
think that’s one of the things that we’re going to be uh be able to say more about and i think we’ll get
more from stream two because stream two is comparing two regiments of the set now comparing two regiments of the same
duration and i think there will be able to uh to unpick that a bit more
so we’ve come to the end um i do want to thank all our panelists very much indeed for joining our
speakers and all of those who have uh joined from across the world listening
great great to have you hope you enjoy the rest of world tv day and i’m going to hand back to peter
our senior um to sign off oh peter’s not available to
close i’m getting a little message from across the socially distanced table here so that falls to me to close then
and and just to say again a thank you picking out really some of the points
that jillian made about the relevance of this work and the relevance of taking forward
things into policy and practice at speed i think we’ve seen that happen in covid and i have a feeling that we should be
able to do better here it strikes me that tuberculosis has already
is always the poor poor neighbor of every other infectious disease it’s been trumped
again by covid even though it’s a respiratory infection and just plays out over slower time
makes worse impacts but i’m hoping we can take these forward together thank you very much everybody
have a good rest of the rest of the day